Natural Ways to Improve Bladder Control and Stop Frequent Urination
Last updated on : 02 Jul, 2025
Read time : 10 min
It begins with a few extra trips to the bathroom. Maybe you’re waking up at night to pee or feeling the urge more often than usual during the day. You brush it off—but it keeps happening.
Frequent urination, medically known as “polyuria,” refers to the need to urinate more often than usual. This can disrupt daily life—interrupting work, sleep, or social activities—and may signal an underlying health condition such as urinary tract infections (UTIs), diabetes, or overactive bladder (OAB) syndrome. Addressing frequent urination is crucial to improving quality of life, achieving restful sleep, and preventing complications.
Lets understand more about overactive bladder syndrome as a significant cause of frequent urination and how to stop frequent urination.
What is Bladder Control?
Bladder control refers to your ability to store urine in the bladder and release it at an appropriate time. It involves coordination between bladder muscles, the nerves that control these muscles, and the muscles that control urine flow out of the bladder.
OAB and urinary incontinence (UI) are two conditions that affect bladder control. While both OAB and UI share symptoms of urgency and frequency, the critical difference is the presence of urine leakage in UI. In an OAB, the muscle contracts involuntarily, causing a sudden and urgent need to urinate. This urgency can occur even when the bladder is not completely filled.
Why does Frequent Urination Occur?
Frequent urination occurs due to an overactive bladder. People with UTIs, nerve damage, bladder infections, bladder stones, and constipation, and those taking diuretic medicines tend to develop OAB and urinate frequently.
OAB can also be a symptom of underlying medical conditions, such as Parkinson’s disease, multiple sclerosis, or diabetes. It is also experienced in pregnancy due to uterus expansion, which puts pressure on the bladder, causing frequent urination.
How to Stop Frequent Urination?
Managing frequent urination naturally involves achieving better bladder control through lifestyle changes, pelvic floor exercises, dietary adjustments, and bladder training techniques. These methods aim to enhance bladder capacity, strengthen supporting muscles, and improve nerve control.
One effective strategy for how to stop frequent urination is to practice pelvic floor exercises, such as Kegels, which can strengthen the muscles that control urination. Lifestyle modifications such as dietary modifications, maintaining a healthy weight, and bladder training techniques support bladder control naturally.
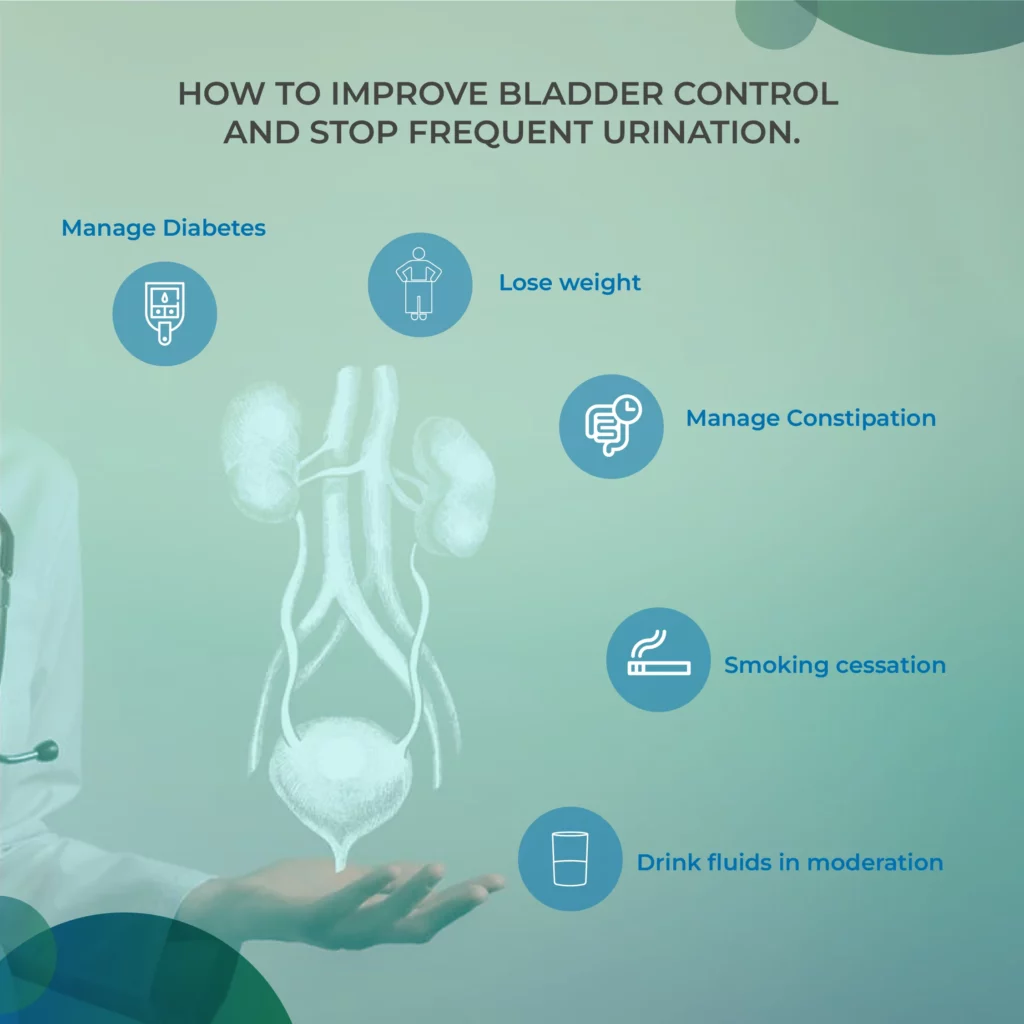
Here are some general considerations that can reduce frequent urination:
1) Drink fluids in moderation
While reducing fluid intake may seem logical, drinking too little water can increase urine concentration and irritate the bladder lining. It’s advisable to maintain a fluid intake of about 1.5 litres per day. To reduce nighttime urination (nocturia), avoid drinking fluids within 3–4 hours before bedtime. Limiting caffeinated and alcoholic beverages is also recommended, as they can irritate the bladder and act as diuretics.
2) Manage Constipation
Being constipated can put pressure on the bladder and cause frequent urination. Therefore, managing constipation by increasing fibre intake, staying hydrated and taking laxatives can help control frequent urination.
3) Lose weight
Excess weight in the abdomen can put pressure on the bladder, causing the urge to empty more frequently than usual. Therefore, reducing excess body weight with physical activity and dietary changes can help prevent frequent urination.
4) Smoking cessation
Smoking can cause chronic coughing, which increases intra-abdominal pressure and worsens urinary symptoms. Smoking cessation reduces the risk of urinary incontinence and improves overall bladder health.
5) Practice pelvic floor exercises
Pelvic floor muscle exercises, such as Kegels, strengthen the muscles that control urination and help manage bladder urgency. These exercises are simple, discreet, and effective for both men and women.
6) Manage Diabetes
Frequent urination is a common symptom of uncontrolled diabetes, especially if your blood sugar levels are consistently high. Managing your diabetes can help you control your frequent urination.
7) Avoid bladder irritants
Certain foods and beverages increase bladder irritability, which triggers OAB symptoms and UI. Caffeine, in particular, has been shown to have a diuretic effect. It is a constituent of a variety of beverages and foods. Caffeine-containing products increase pressure on the bladder, which causes frequent urination. Therefore, avoiding caffeine products can reduce frequent urination.
Besides caffeine, eliminating the following foods from the diet can also reduce frequent urination.
- Spicy foods
- Artificial sweeteners
- Chocolate
- Citrus fruits
- Corn syrup
- Cranberry juice
- Carbonated drinks
- Refined sugar
- Tomatoes
- Vinegar
8) Herbs and supplements for overactive bladder
Some herbs and supplements for managing an overactive bladder include:
- Saw Palmetto
- Pumpkin Seed Extract
- Gokshura
- Ashwagandha
- Shatavari
- Cranberry Extract
- Magnesium
- Horsetail
- Resiniferatoxin
- Capsaicin
- Corn silk
- Cleavers
Pumpkin seed extract and saw palmetto are especially promising based on current evidence. However, you should consult a healthcare provider before starting any supplements, particularly if you are already on medications or have chronic health conditions.
Scheduling bathroom visits can also train your bladder naturally to hold more urine and reduce the frequency of urination.
If you experience painful urination, blood in the urine, or fever, it’s best to consult your doctor to avoid complications.
Exercises to Control Frequent Urination
Pelvic floor muscle strengthening is considered first-line treatment for overactive bladder and urinary incontinence. These exercises help reinforce the muscles supporting the bladder and urethra, improving control and reducing urgency.
Here are some exercises for bladder control.
1. Kegels
Kegel exercises involve contraction and relaxation of the muscles that control urine flow. To perform Kegels, sit or lie down and squeeze the pelvic floor muscles for 5-10 seconds, then relax simultaneously. Repeat this 10-15 times, three times a day.
Avoid holding your breath or tensing your abdominal or thigh muscles while performing Kegel contractions, and focus on contracting only the pelvic floor muscles.
2. Squats
Squats strengthen the pelvic floor muscles and improve bladder control. Squats are performed by standing with your feet shoulder-width apart, bending your knees, and lowering your body as if you were sitting. Return to standing and repeat for 10-15 repetitions thrice daily.
3. Bridge pose
It’s a yoga posture to strengthen the pelvic floor muscles. To perform bridge pose:
- Lie on your back with legs bent and feet flat.
- Lift your hips toward the ceiling, squeezing your glutes and pelvic floor muscles.
- Hold for 5-10 seconds, then release and repeat thrice daily for 10-15 repetitions.
4. Pelvic tilts
Pelvic tilts involve tilting the pelvis forward and backwards to engage the pelvic floor muscles. To perform pelvic tilts:
- Lie on your back with legs bent and feet flat.
- Pull your abdominal muscles tight and tilt your pelvis forward, then release and tilt it backward.
- Repeat 10-15 repetitions three times a day.
Bladder Control Techniques
Bladder training helps increase the time between urination and reduce urgency. This technique may take weeks to months but can be highly effective when done consistently.
1. Scheduling bathroom visits
Begin by urinating every 30 minutes, whether or not you feel the urge. Gradually extend the time between visits to 3–4 hours. This allows your bladder to hold more urine comfortably. You can start with 30-minute intervals, then increase to 45-minute intervals, then 1-hour intervals, and so on until a voiding interval of at least 3–4 h is achieved.
2. Delay urination
If you feel the urge to urinate, try delaying it for a few minutes, then slowly increase the delay time. This helps improve your bladder’s capacity and control.
3. Double void technique
The double void technique suggests fully emptying the bladder and reducing the need to urinate frequently. It involves urinating, waiting a few minutes, and then trying to urinate again to ensure that your bladder is fully emptied. When you feel the urge to urinate, go to the bathroom as usual. Then, wait for 3 to 5 minutes and try to urinate again. It ensures that the bladder is fully empty and reduces your urge to urinate again shortly after.
Diet for Bladder Control
Diet plays a crucial role in supporting bladder health. Avoiding bladder irritants and including certain nutrient-rich foods can improve bladder control.
Foods that support bladder health:
1. Leafy greens
Leafy greens such as spinach, mustard greens, and fenugreek leaves are high in vitamin C and magnesium, which can help support bladder health.
2. Whole grains
High fibre foods like quinoa, brown rice, barley, oats, and barn can help prevent constipation and promote regular bowel movements.
3. Lean proteins
Lean proteins such as eggs, chicken, fish, and tofu help support pelvic muscle strength for bladder control.
4. Yoghurt
Yogurt contains probiotics, which balances gut bacteria and prevents UTIs
5. Berries
Berries, such as blueberries, raspberries, and strawberries, are rich in antioxidants and can reduce bladder inflammation.
6. Almonds
Almonds are a good source of magnesium, which plays a crucial role in muscle function and nerve signalling to control frequent urination. It also reduces bladder irritability and improves bladder control.
7. Bananas
Bananas are a good potassium source, which regulates fluid balance in the body and maintains muscle function to improve bladder control.
A registered dietitian can help you create a personalized diet plan tailored to your needs and preferences.
Conclusion
While an overactive bladder may not be curable in all cases, symptoms of frequent urination can be managed effectively with lifestyle modifications, bladder training, pelvic floor exercises, and dietary changes. If natural strategies are not sufficient, consult a urologist, gynaecologist, or urogynecologist for further evaluation and treatment.
You can also manage your treatment through Truemeds by uploading your prescription and availing free teleconsultation with expert doctors. Download the Truemeds app to get genuine medicines and save up to 72% by choosing recommended alternatives.
Frequently Asked Questions
Foods rich in fibre, protein, magnesium, and potassium can stop frequent urination. Include bananas, apples, grapes, watermelons, and berries in your diet. Also add vegetables, such as leafy greens, carrots, cucumbers, peppers, and whole grains such as oats, quinoa, and brown rice .
To stop frequent urination, you must limit your water intake to 1.5 lt daily. It’s also recommended to reduce fluid intake in the evening—about 3–4 hours before bedtime—to help prevent nocturia (frequent nighttime urination).
However, drinking less fluids can make your urine concentrated and cause irritation to the lining of your urinary tract.
You can manage frequent urination naturally through a combination of dietary modifications (e.g., increased fibre intake), avoiding known bladder irritants, practising pelvic floor exercises like Kegels, and implementing bladder control techniques such as bladder training and scheduled voiding.
Common medications used to manage overactive bladder in men include alpha-blockers (e.g., Tamsulosin, Alfuzosin) and anticholinergics (e.g., Oxybutynin, Tolterodine). These medications help relax bladder muscles and reduce urgency, frequency, and leakage. Always consult a doctor before starting any medication.
With consistent treatment—whether through lifestyle changes, medications, or both—overactive bladder symptoms can improve within 6 to 12 months. However, the timeline can vary depending on the individual and the underlying cause.
References
- https://www.sciencedirect.com/science/article/pii/S2772973725000062
- https://www.sciencedirect.com/science/article/pii/S277297372300142X
- https://www.sciencedirect.com/science/article/pii/S2772974522000047
- https://onlinelibrary.wiley.com/doi/10.1111/iju.14663
- https://jurnal.globalhealthsciencegroup.com/index.php/IJGHR/article/view/5242
- https://journals.lww.com/jpbs/fulltext/2025/05001/effect_of_exercise_regimen_on_stress_urinary.85.aspx
Disclaimer
Our healthcare experts have carefully reviewed and compiled the information presented here to ensure accuracy and trustworthiness. It is important to note that this information serves as a general overview of the topic and is for informational purposes only. It is not intended to diagnose, prevent, or cure any health problem. This page does not establish a doctor-patient relationship, nor does it replace the advice or consultation of a registered medical practitioner. We recommend seeking guidance from your registered medical practitioner for any questions or concerns regarding your medical condition.
Popular Articles
Recommended Articles
Recent Articles
Company
About UsHealth ArticleHealth StoriesDiseases & Health ConditionsAyurvedaAll MedicinesAll BrandsNeed HelpFAQSubscribe
Registered Office Address
Grievance Officer
Download Truemeds
Contact Us
Our customer representative team is available 7 days a week from 9 am - 9 pm.
v4.3.8
2025 - Truemeds | All rights reserved. Our content is for informational purposes only. See additional information.
Our Payment Partners



















































